Estimated reading time: 8 minutes
Key Takeaways
- The Whipple procedure is the most effective surgical treatment for localized pancreatic cancer.
- Only 20-25% of patients are candidates for this complex surgery due to disease progression.
- Five-year survival rates reach 20-25% for those who undergo successful resection.
- Recovery requires 8-12 weeks with significant lifestyle adjustments and ongoing care.
- Treatment at high-volume centers significantly improves outcomes and reduces complications.
Table of contents
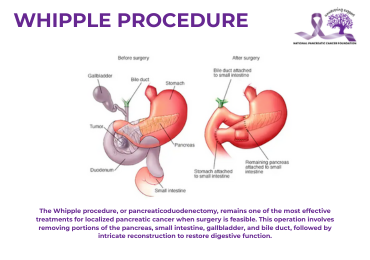
The Whipple procedure, or pancreaticoduodenectomy, remains one of the most effective treatments for localized pancreatic cancer when surgery is feasible. This operation involves removing portions of the pancreas, small intestine, gallbladder, and bile duct, followed by intricate reconstruction to restore digestive function.
While complex, advances in surgical techniques have improved safety and outcomes significantly since the procedure’s inception. This guide clarifies what patients and families should know about candidacy, recovery, and long-term adjustments after Whipple surgery.
What Is the Whipple Procedure?
The Whipple procedure targets tumors in the head of the pancreas, which accounts for most pancreatic cancer cases. Surgeons remove:
- The pancreas’s head
- The duodenum (first part of the small intestine)
- The gallbladder and bile duct
- Occasionally, part of the stomach
The remaining organs are then reconnected to preserve digestion. Though originally developed in the 1930s, modern refinements including minimally invasive approaches at some centers, have enhanced precision and reduced complications. For additional context on surgical strategies, readers may wish to review our article on Pancreatic Cancer: Surgery and Chemotherapy Options.
This surgery may also address conditions like neuroendocrine tumors, chronic pancreatitis, or cancers of the bile duct or duodenum when localized.
Key Resources:
• Johns Hopkins Medicine: Whipple Procedure
• Cleveland Clinic Overview
Surgical Eligibility for Pancreatic Cancer
Not all pancreatic cancer patients qualify for resection. Surgery is typically reserved for cases where:
- The tumor is confined to the pancreas
- Critical blood vessels are unaffected
- No distant metastases (e.g., to the liver or lungs) are present
- The patient’s overall health can withstand major surgery
For stage 4 pancreatic cancer (metastatic disease), systemic therapies like chemotherapy are standard. However, multidisciplinary teams may consider surgery in rare instances, such as oligometastatic cases within clinical trials. Patients interested in understanding the full spectrum of treatment avenues can also explore our Pancreatic Cancer Treatment Guide: Options and Advocacy.
Survival Outcomes After Surgery
Five-year survival rates post-Whipple hover around 20–25% for localized disease, significantly higher than non-surgical options. Outcomes improve with:
- Earlier-stage diagnoses (Stage 1 tumors have better prognoses)
- Complete tumor removal (“negative margins”)
- Treatment at high-volume centers (experienced surgeons yield better results)
- Adjuvant therapies like chemotherapy
While statistics provide benchmarks, individual factors such as tumor biology, age, and response to treatment play pivotal roles in long-term survival.
Recovery and Post-Operative Care
Immediate Recovery (Hospital Stay)
- 1–2 weeks of hospitalization, starting in intensive care
- Gradual reintroduction of fluids and foods
- Pain management and mobility assistance
Long-Term Adjustments
- Digestive changes: Smaller, frequent meals; enzyme supplements for some
- Monitoring for complications: Diabetes, malabsorption, or infections
- Emotional and physical support: Fatigue may persist for months
For supportive nutritional guidance during recovery, consider reading our article on Juicing Benefits and Nutritional Insights for Health.
Caregivers should watch for warning signs like fever, jaundice, or severe pain and assist with medication management and nutrition.
Pre-Surgery Preparation
Medical Readiness
- Imaging (CT/MRI) and bloodwork to assess candidacy
- Cardiac and anesthesia evaluations
Practical Steps
- Arrange 8–12 weeks for recovery
- Secure home support for meals, transportation, and follow-ups
- Pack essentials for the hospital: loose clothing, medications, personal items
Psychological preparation through counseling or peer support can ease pre-surgery anxiety. In addition, adopting a proper diet is crucial before surgery; you might find valuable information in our guide Diet Tips For Pancreatic Cancer Patients.
Weighing Risks and Benefits
Potential Complications
- Infections, bleeding, or leaks at surgical sites
- Delayed gastric emptying (30% of cases)
- New-onset diabetes or nutritional deficits
Advantages
- Potential for cure in localized disease
- Symptom relief (e.g., reducing bile duct obstruction)
- Extended survival compared to non-surgical treatments
High-volume centers report lower complication rates, underscoring the importance of surgeon experience.
Support and Resources
Patients and caregivers can access:
- Medical teams: Dietitians, social workers, and physical therapists
- Support groups: NPCF-led networks or hospital-based programs
- Financial aid: Insurance navigation and transportation assistance
For comprehensive assistance, both emotional and medical, explore our resource page on Pancreatic Cancer Support: Emotional & Medical Resources. One survivor noted:
“Connecting with others who’d been through this helped normalize the challenges.”
Frequently Asked Questions
Who qualifies for the Whipple procedure?
Patients with localized tumors, no major vascular involvement, and sufficient health to endure surgery.
Can stage 4 pancreatic cancer be treated surgically?
Rarely. Chemotherapy is the primary approach for metastatic disease.
How long is recovery?
Most resume normal activities within 3 months, though full recovery may take longer.
What’s the survival rate after surgery?
Approximately 20–25% at 5 years for eligible patients, with better outcomes at specialized centers.