Estimated reading time: 7 minutes
Key Takeaways
- Pancreatic cancer has a five-year survival rate of just 13%, making early detection crucial
- 5-10% of cases are hereditary, linked to mutations in genes like BRCA1, BRCA2, and others
- Lifestyle factors like smoking, obesity, and diabetes significantly increase risk
- Smoking cessation is the most impactful modifiable prevention strategy
- Genetic counseling and testing can help identify high-risk individuals
Table of contents
Introduction
Pancreatic cancer remains one of the most challenging malignancies to treat, with a five-year survival rate of just 13%. In 2023 alone, approximately 64,050 Americans will receive a pancreatic cancer diagnosis. The disease’s aggressive nature and late-stage detection (learn more about recognizing early signs) contribute to its poor prognosis, making awareness of its causes essential for prevention and early intervention.
What Causes Pancreatic Cancer
Pancreatic cancer originates when pancreatic cells mutate and proliferate uncontrollably. Over 90% of cases involve pancreatic ductal adenocarcinoma (PDAC), which develops in the ducts responsible for transporting digestive enzymes.
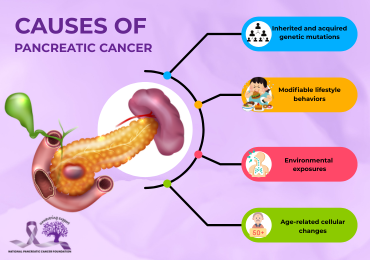
The disease stems from multiple contributing factors:
- Inherited and acquired genetic mutations
- Modifiable lifestyle behaviors
- Environmental exposures
- Age-related cellular changes
While most diagnoses lack a single identifiable cause, research has established clear correlations between certain risk factors and disease development. These elements often interact cumulatively over time, creating conditions favorable for cancer progression.
Genetic Predisposition to Pancreatic Cancer
Approximately 5–10% of pancreatic cancer cases are hereditary, linked to gene mutations passed through families. Hereditary cases typically present distinct patterns:
- Earlier onset than sporadic cases
- Multiple affected relatives across generations
- Higher prevalence in specific ethnic populations
- Associations with other inherited cancer syndromes
Key genes associated with increased risk include:
- BRCA1/BRCA2: Primarily linked to breast and ovarian cancers but also elevate pancreatic cancer risk
- PALB2, ATM: DNA repair genes
- CDKN2A: Regulates cell cycle progression
- STK11: Associated with Peutz-Jeghers syndrome
- Lynch syndrome genes (MLH1, MSH2, MSH6, PMS2)
Individuals with two or more first-degree relatives affected by pancreatic cancer face a 5–7 times higher risk than the general population. For a comprehensive overview of pancreatic cancer, expert resources are available.
The BRCA Connection
BRCA1 and BRCA2 mutations impair DNA repair mechanisms, increasing susceptibility to multiple cancer types. Regarding pancreatic cancer:
- 5–7% of patients carry BRCA or other high-risk mutations
- BRCA2 mutations confer the highest risk (3–5 times baseline)
- BRCA1 mutations double the risk
These genetic links have clinical implications:
- PARP inhibitor therapies show efficacy against BRCA-mutated tumors
- High-risk families may qualify for enhanced screening protocols
- Genetic testing informs preventive strategies for mutation carriers
For more information on treatment options and genetic insights, expert guidance is available for patients and families.
Modifiable Risk Factors
Lifestyle choices significantly influence pancreatic cancer risk. The most consequential factors include:
Tobacco Use
- Responsible for 20–30% of cases
- Current smokers face 1.5–2 times higher risk
- Risk correlates with smoking duration and intensity
- Cessation reduces risk gradually over 10–15 years
Metabolic Factors
- Obesity: BMI >30 increases risk by 20%
- Type 2 diabetes: Associated with 1.5–2 times higher risk
- Chronic pancreatitis: Long-term inflammation elevates risk
Additional Lifestyle Considerations
- Diet: High processed meat intake may increase risk; plant-rich diets appear protective (for more detailed diet recommendations, expert guidance is available).
- Alcohol: Heavy consumption (>3 drinks/day) raises pancreatitis risk
- Activity: Sedentary lifestyles correlate with higher incidence
Additionally, integrating nutritional practices such as juicing may further support overall dietary health (discover more about juicing benefits for comprehensive nutrition strategies).
Prevention Strategies
Effective risk reduction involves:
- Smoking cessation: Eliminates a major reversible risk
- Weight management: Achieving and maintaining healthy BMI
- Diabetes control: Monitoring blood sugar levels
- Dietary optimization: Emphasizing fruits, vegetables, and whole grains
- Physical activity: 150+ minutes of exercise weekly
- Genetic counseling: For families with clustering of cases“Prevention is the most powerful weapon we have against pancreatic cancer. Understanding your personal risk factors empowers you to make informed decisions about your health.”
Conclusion
Pancreatic cancer develops through complex interactions between genetic susceptibility and environmental exposures. While hereditary factors account for a minority of cases, lifestyle modifications present meaningful opportunities for prevention. Awareness of risk factors, particularly smoking cessation and metabolic health, empowers individuals to mitigate their disease risk.
For those with familial predisposition, genetic counseling and targeted screening offer additional protective measures. The key to fighting this challenging disease lies in early awareness, risk reduction, and proactive healthcare engagement.
Frequently Asked Questions
Is pancreatic cancer survivable?
Survival depends heavily on early detection. Localized tumors have significantly better outcomes than metastatic disease.
How often is pancreatic cancer inherited?
5–10% of cases stem from hereditary gene mutations.
Who should consider genetic testing?
Individuals with ≥2 close relatives with pancreatic cancer or one relative diagnosed before age 50.
Can lifestyle changes prevent pancreatic cancer?
Yes, particularly through smoking avoidance, weight management, and dietary modifications.
What symptoms warrant medical evaluation?
Unexplained weight loss, jaundice, new-onset diabetes after age 50, or persistent abdominal pain.