Estimated reading time: 12 minutes
Key Takeaways
- The Whipple procedure is a complex surgery that removes the head of the pancreas and surrounding organs to treat pancreatic cancer.
- Recovery requires patience and careful management, with hospital stays typically lasting 7-14 days followed by months of gradual healing.
- Most patients will need pancreatic enzyme supplements and dietary modifications for optimal digestion post-surgery.
- Five-year survival rates range from 20-30% for pancreatic adenocarcinoma, but individual outcomes vary significantly.
- Preparing questions for your surgical team and seeking comprehensive support are crucial for navigating this journey successfully.
Table of contents
A diagnosis involving the pancreas often leads to a discussion about a complex operation known as the Whipple procedure. For patients and their families, this moment can feel overwhelming, marked by a flood of questions about the surgery itself and the road that follows. This guide provides a clear, detailed overview of the Whipple procedure, from the operating room through recovery and long-term outcomes. Our goal is to equip you with knowledge, helping to transform uncertainty into understanding and preparation.
What Is the Whipple Procedure?
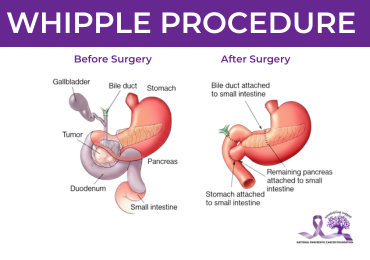
Medically termed a pancreaticoduodenectomy, the Whipple procedure is a major abdominal operation to remove tumors located in the head of the pancreas. To ensure complete removal of the cancer, surgeons also remove:
- The duodenum (the first part of the small intestine)
- The gallbladder
- A portion of the bile duct
- Occasionally, a part of the stomach
The remaining digestive organs are then carefully reconnected to restore function.
This surgery is most commonly indicated for cancers that originate in the head of the pancreas, the distal bile duct, or the ampulla of Vater. It is considered when the tumor appears confined to the area and has not spread to distant organs or extensively involved critical local blood vessels.
A patient’s eligibility hinges on several factors. Surgeons assess the tumor’s size and location through advanced imaging, confirm there is no distant metastasis, and evaluate the patient’s overall health to ensure they can withstand a significant operation. For more on the tests and imaging used to evaluate pancreatic tumors, comprehensive diagnostic workups are essential.
In some cases, chemotherapy or radiation may be recommended before surgery to shrink the tumor and improve the chances of a successful resection. For detailed information about chemotherapy options and how they may be used around the time of surgery, understanding these treatments can help prepare you for the complete treatment journey.
What to Expect During the Operation
The Whipple procedure is performed under general anesthesia and typically lasts between five and eight hours. The surgical approach is tailored to the individual patient. The traditional method is an open surgery, involving a single vertical incision to provide the surgical team with direct access and visualization.
For select patients, a minimally invasive approach, using laparoscopic or robotic techniques through several small incisions, may be an option. This can sometimes lead to reduced blood loss and a shorter initial recovery, though it requires a highly specialized surgical team and is not suitable for every case due to tumor characteristics or patient anatomy.
The operation follows a meticulous sequence:
- Exploration: The surgeon explores the abdomen to confirm the cancer has not spread
- Resection: The affected organs are removed
- Reconstruction: The digestive system is carefully rebuilt
The reconstruction involves connecting the remaining pancreas, bile duct, and stomach to the small intestine so digestive juices and food can flow properly.
“Throughout the procedure, the team’s priority is achieving a resection with ‘clear margins,’ meaning no cancer cells are left at the edges of the removed tissue.”
The pathologist examines tissue samples during the surgery to help guide this effort.
Recovery Timeline: Hospital to Home
Recovery from a Whipple procedure is a phased process, requiring patience and careful management.
Initial Hospital Stay (7-14 days)
The initial hospital stay generally ranges from seven to fourteen days. During this time, the focus is on:
- Managing pain effectively
- Preventing complications
- Gradually restarting basic bodily functions
Patients are encouraged to sit up and take short walks very soon after surgery, which helps prevent blood clots and pneumonia. Tubes placed during surgery, such as those draining fluids from the abdomen or temporarily decompressing the stomach, are removed as recovery progresses.
Two of the most common early complications are delayed gastric emptying, where the stomach takes longer than usual to move food forward, and leakage from the newly created connections between organs. Your care team monitors closely for these issues.
Home Recovery (Several Weeks)
Upon returning home, the next several weeks involve continued healing. Energy levels may be low, and a gradual return to activity is advised. For practical tips on managing fatigue and gradually increasing activity after major pancreatic surgery, understanding energy management is crucial.
Dietary changes are central to this phase. Most patients start with easily digestible liquids and soft foods, slowly advancing their diet as tolerated. Because a portion of the pancreas is removed, some patients experience difficulty digesting fats and proteins. This condition, called exocrine pancreatic insufficiency, may require taking prescribed pancreatic enzyme supplements with meals to aid nutrition and prevent weight loss.
For guidance on nutrition and managing digestive changes after pancreatic surgery and practical meal planning ideas, working with a specialized dietitian becomes invaluable.
Long-term Recovery (Several Months)
Long-term recovery, spanning months, involves regaining strength, adapting to any lasting dietary needs, and resuming normal activities. Follow-up appointments are crucial to monitor healing, manage any new medications, and begin any recommended additional treatments like chemotherapy.
Risks, Complications, and Quality of Life
As with any major operation, the Whipple procedure carries risks. Beyond the common early complications mentioned, there are risks of bleeding, infection, and reactions to anesthesia. Long-term considerations are important for ongoing quality of life.
A significant number of patients will require lifelong pancreatic enzyme replacement therapy to digest food properly. There is also a risk of developing diabetes after surgery, as the insulin-producing cells in the removed portion of the pancreas are lost. This occurs in a minority of patients but requires careful monitoring and management.
Despite these challenges, many people achieve a good quality of life post-surgery. Successful management of digestive and endocrine changes allows patients to return to work, hobbies, and family life. Working closely with a dietitian, an endocrinologist if needed, and your surgical oncologist is key to navigating this adaptation.
If you’re weighing surgical options or want to understand how the Whipple compares with other approaches, see our treatment options guide for comprehensive information about making informed treatment decisions.
Understanding Survival Rates
Survival statistics following a Whipple procedure are inherently general and should be viewed as one piece of a much larger picture. For pancreatic adenocarcinoma, the most common type of pancreatic cancer, five-year survival rates after successful resection are often cited between 20% and 30%.
It is vital to understand what these numbers represent: they are population averages that include a wide range of individual experiences.
“Your personal prognosis is influenced by factors that no broad statistic can capture.”
The most important factors include:
- The specific cell type of the cancer
- The stage at diagnosis
- Whether the cancer had spread to lymph nodes
- Whether surgeons achieved completely clear margins
- Your overall health and response to follow-up treatments
The most meaningful conversation about survival will be with your own oncology team, who can interpret your unique situation.
For broader context on life after pancreatic cancer and survivorship issues, including monitoring and long-term challenges, comprehensive support continues beyond initial treatment.
Whipple Procedure vs. Total Pancreatectomy
In certain situations, a surgeon may determine that a total pancreatectomy, removing the entire pancreas, is necessary instead of a Whipple. This decision is typically based on the extent of the tumor. If cancer involves a large portion of the pancreas or is multifocal, preserving part of the organ may not be safe or oncologically sound.
The functional consequences of a total pancreatectomy are significant. Because the entire pancreas is removed, the patient will:
- Inevitably develop insulin-dependent diabetes
- Absolutely require pancreatic enzyme replacement therapy
- Face a more complex recovery process
The choice between these procedures is not a matter of patient preference but a surgical judgment made to offer the best chance of a cure, balancing the need to remove all cancer with the goal of preserving as much function as possible.
If you want more detail on when each surgical option is recommended and how to discuss these choices with your team, review our treatment options guide for comprehensive decision-making support.
Questions for Your Surgical Team
Preparing a list of questions can help you feel more in control and ensure you get the information you need. Consider asking your surgeon:
- What is your personal and institutional experience with this specific operation?
- Based on my scans, how likely are you to achieve a complete resection?
- What is the possibility of beginning the Whipple but needing to convert to a total pancreatectomy?
- What are the most common complications you see at your center?
- How will we manage my pain and nutrition after surgery?
- What is the planned follow-up, and when would adjuvant therapy like chemotherapy begin?
For additional suggested questions specifically for oncologists and treatment planning, comprehensive preparation helps ensure productive discussions with your care team.
Support and Resources
Navigating this journey does not have to be a solitary endeavor. Seek support early. Organizations like the National Pancreas Foundation offers extensive resources, including:
- Patient education materials
- Dietetic advice specialized for pancreatic conditions
- Support group connections
- Clinical trial navigation
Asking your hospital’s oncology social worker for local resources can also be invaluable. For a curated list of emotional and medical support resources, comprehensive assistance is available throughout your journey.
The Whipple procedure is a formidable yet potentially life-saving operation. While the path through diagnosis, surgery, and recovery is demanding, understanding the process demystifies it. Armed with knowledge about what the surgery entails, what a realistic recovery looks like, and how to manage long-term health, patients and families can move forward with greater confidence.
“Remember that your medical team is your partner, and seeking comprehensive support can profoundly impact your experience and outcome.”
Frequently Asked Questions
How long does the Whipple procedure take?
The Whipple procedure typically takes between five and eight hours to complete. The exact duration depends on factors such as the complexity of your specific case, the surgical approach used, and whether any complications arise during the operation.
Will I be able to eat normally after a Whipple procedure?
Most patients can eventually return to eating a relatively normal diet, though modifications are often necessary. You may need to take pancreatic enzyme supplements with meals to help digest food properly, and you’ll likely need to eat smaller, more frequent meals initially. Working with a dietitian is essential for optimal nutrition management.
What is the difference between open and minimally invasive Whipple surgery?
Open surgery involves a single larger incision for direct access, while minimally invasive approaches use several small incisions with laparoscopic or robotic techniques. Minimally invasive surgery may offer reduced blood loss and shorter initial recovery for select patients, but it’s not suitable for all cases and requires highly specialized surgical expertise.
How soon after surgery can I return to normal activities?
Recovery is gradual and varies by individual. Most patients can begin light activities within a few weeks, but full recovery typically takes several months. You’ll start with short walks in the hospital and gradually increase activity levels as your body heals. Your surgical team will provide specific guidelines based on your progress.
Will I develop diabetes after a Whipple procedure?
Some patients do develop diabetes after the Whipple procedure because insulin-producing cells in the removed portion of the pancreas are lost. This occurs in a minority of patients and requires careful monitoring. If diabetes develops, it can typically be managed effectively with medication and dietary modifications.